The sciatic nerve is massive. It’s both the longest and thickest nerve in the human body. It’s also among the body’s most notorious nerves. With up to 40 percent of people experiencing sciatica at some point in their life, the name of this nerve has made its way into everyday vocabulary.¹ Compression at the level of spinal discs, where the sciatic nerve exits the spinal canal, or further down, where the nerve passes by a potentially spasming piriformis, are both well-established causes of sciatica. Yet irritation at any point along this lengthy nerve can trigger painful sciatica symptoms.
As bodyworkers, we’re familiar with sciatica, but when we study the nerve itself, we often see only a partial picture that focuses on its lengthy longitudinal path (Image 1). That view tells us where compression might occur, but this big nerve has a bigger story—a fascia story. As the understanding of fascia evolves, researchers are recognizing neural fascia—the connective tissues both within and surrounding nerves—as an integral part of the broader fascial system.²
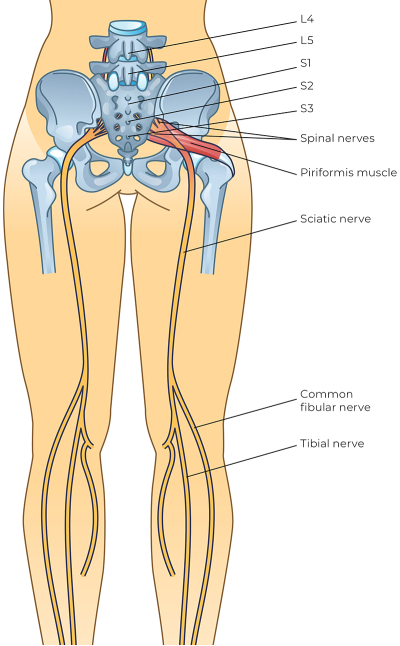
By examining both the sciatic nerve’s internal connective tissue architecture and external fascial relationships, we rediscover it as a dynamic 3D structure that depends on its fascial connections for healthy function—from the inside out.
Looking In: More Than Nerve
Looking inside the sciatic nerve, we discover that the nerve is not all nerve. Certainly, we find neurons and their supporting glial cells. These cells are specialized to do the work of the nervous system, enabling communication through rapidly transmitting electrochemical impulses. But we also see layers of connective tissue organizing the neural components in a hierarchical structure:
-
Endoneurium (around individual nerve fibers)
-
Perineurium (surrounding bundles of nerve fibers)
-
Epineurium (encasing the bundles of bundles, forming an outer sheath around the entire nerve).
If endo-, peri-, and epi- sound familiar, it’s because we find a similar hierarchical organization of connective tissue in muscle.³ These layers of connective tissue stabilize the nerve and allow individual components within the nerve to slide in relation to each other (Image 2). This is an important detail. Even though the sciatic nerve is protected deep within the tissues, it is regularly subjected to shearing and compressing forces as the body moves, sits, and stretches. The nerve’s internal organization allows each component to slide and distort just enough to accommodate the movement of bodies in a frictionless manner.
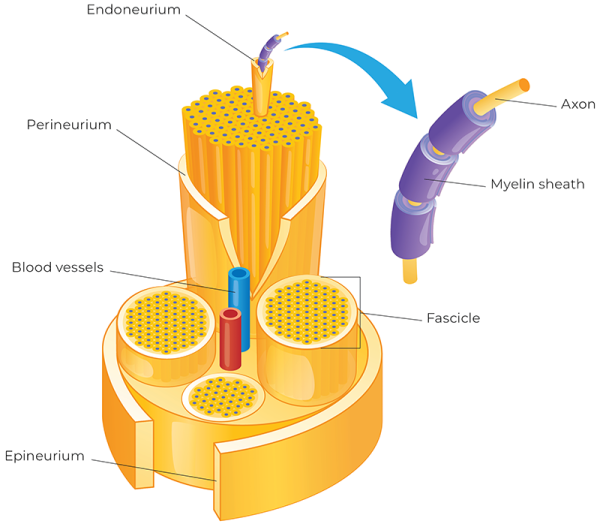
The outermost layer, the epineurium, establishes the nerve’s relationship with surrounding tissues. This layer of dense connective tissue forms a smooth surface that works in conjunction with the paraneurium—a cloud of lubricating loose connective tissue that surrounds peripheral nerves, allowing them to glide friction-free against surrounding structures. This complementary arrangement of “smooth dense” and “slippery loose” connective tissues creates a perfect interface for the nerve to slide and glide. When this gliding mechanism is compromised—whether through adhesions, inflammation, or mechanical restrictions—the nerve becomes vulnerable to tension, compression, and friction, potentially resulting in pain.
The [sciatic] nerve’s internal organization allows each component to slide and distort just enough to accommodate the movement of our bodies in a frictionless manner.
While techniques such as nerve flossing target the nerve itself, as bodyworkers, we work with nerves in their broader anatomical context, touching entire limbs (skin, fat, fascia, muscle, and bone) rather than isolated structures.4 To understand this more holistic context, let’s examine the deep fascia of the thigh to see where the sciatic nerve lives and travels.
Looking Out: Good Neighbors
Just beneath the skin and subcutaneous fat, we find the deep fascia. This collagen-rich, fibrous tissue encases each of the limbs like a long sleeve or pair of yoga leggings. On the thigh, this enveloping deep fascia is called the fascia lata.5 At first glance, the fascia lata appears to be just a membrane wrapping around the thigh muscles, almost like plastic wrap. When viewed in cross-section, it reveals itself as a 3D structure: from the fascia lata’s inner surface, walls of connective tissue (septa) dive deep to the bone, merging with the femur’s periosteum at the linea aspera. The septa create three fascial compartments: anterior (quadriceps), posterior (hamstrings), and medial (adductors). These compartments act as functional divisions for the muscles, allowing for coordinated movement (Image 3).
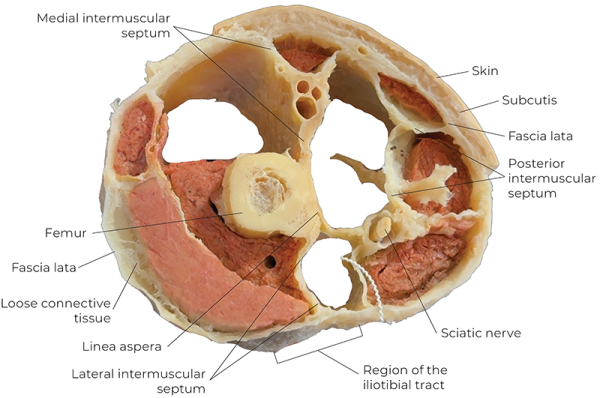
Safe Passage
The septa do more than organize muscles; they provide passage and structure for our deep blood vessels and nerves, including the sciatic nerve. The fascial septa create a tubular opening, or sheath, for the sciatic nerve to travel the length of the femur. This sheath is not so evident when we study the sciatic nerve only along its longitudinal path, but when we shift our perspective to a cross-sectional view, it becomes more apparent. Inside this sheath, we find the sciatic nerve with its smooth epineurium and the slippery cloud of paraneurium, allowing the nerve to slide friction-free against the walls. Free to glide, the nerve can adapt to our constant movements and tissue distortions without being overly stretched or compressed. Friction-free gliding is essential, but the nerve also relies on another set of neighbors to maintain the integrity of its home: muscles!
Tense Neighbors
You won’t find this in most of your anatomy books (we checked!), but the fascia lata also serves as an insertion point for the muscles of the thigh. What does this look like? Individual muscle fibers insert into the fascia lata, including the septa. When these muscles contract, they don’t just pull on their bony attachments; they also pull directly on the three-dimensional deep-fascia framework. In this way, the muscles tension the septa of the fascial compartment every time they contract. This helps optimize force transmission, and it might also help keep the sciatic nerve healthy (see accompanying video).
Every time our muscles tension the septa, they also tension the sciatic nerve’s fascial sheath from all sides. This anatomical arrangement cleverly ensures that our contracting muscles maintain the nerve’s protective sheath instead of compressing it. But it also means that imbalances in muscle tone or restrictions in the fascia can create distortions or narrowing of this sheath, preventing the nerve from gliding in the middle and creating friction or irritation.
Why We Care
The sciatic nerve’s story is incomplete without considering its 3D fascial reality—from its internal sliding mechanisms to its fascial environment. This wider perspective reveals how sciatic symptoms can emerge from multiple sources: compromised mobility in gliding relationships, restrictions within fascial compartments, or muscular imbalances that distort the nerve’s protective sheath.
For clients who haven’t found relief through traditional methods focused solely on disc compression or piriformis syndrome, we can potentially develop more approaches to sciatic pain by working with these tissue relationships. For us as bodyworkers, this means expanding our focus beyond the nerve itself to address its entire neighborhood.
Notes
1. M. A., Stafford, P. Peng, and D. A. Hill, “Sciatica: A Review of History, Epidemiology, Pathogenesis, and the Role of Epidural Steroid Injection in Management,” British Journal of Anaesthesia 99, no. 4 (October 2007): 461–73, https://doi.org/10.1093/bja/aem238.
2. Carla Stecco et al., “Towards a Comprehensive Definition of the Human Fascial System,” Journal of Anatomy (January 2025), https://doi.org/10.1111/joa.14212.
3. Muscle tissue is organized by connective tissue in a similar hierarchy of endomysium, perimysium, and epimysium.
4. Nerve flossing aims to restore the gliding relationship along a particular nerve’s path, reducing any restrictions that might be irritating the nerve or causing pain.
5. The lateral part of the fascia lata is thickened, forming the IT band. See “Fascia Lata: Home of the IT Band,” Massage & Bodywork 38, no. 2 (March/April 2023): 66–9, https://www.abmp.com/massage-and-bodywork-magazine/fascia-lata-home-it-band.
Resource
Smoll, N. R. “Variations of the Piriformis and Sciatic Nerve with Clinical Consequence: A Review.” Clinical Anatomy 23, no. 1 (January 2010): 8–17. https://doi.org/10.1002/ca.20893.








