The World Health Organization estimates that 90 percent of low-back pain is “nonspecific,” meaning the pain is not connected to a known disease or structural problem.¹ Perhaps even more concerning, by some estimates, up to 84 percent of the population will experience low-back pain within their lifetime. All that adds up to a lot of people who have back pain without an obvious reason. What’s going on? How can that many people be suffering and not know why?

If it’s not a structural issue and the discs, muscles, and nerves are not the source, where is it coming from? Researchers are looking to another tissue that might have more responsibility in healthy, pain-free function of the low back than previously considered: the thoracolumbar fascia (TLF).
A Multilayered Hub
Starting with a macro view, we look beneath the skin and subcutaneous fat, where we find the TLF superficial to the muscles. When you palpate the muscles of the low back and sacrum, you feel fascia first, more superficially. Fascia is often described as the tissue that envelops muscles like the skin of a sausage, but fascia has more than one type. Each muscle has its own epimysium, akin to sausage skin. But a tougher, stronger fascial structure called aponeurotic fascia can also be found connecting groups of muscles throughout the body. In the low back, we find a famous aponeurotic fascia that is created by the convergence of multiple muscles’ overlapping flat tendons (or aponeuroses), forming a tough, white, diamond-shaped hub: the TLF (Image 1).
The collagen fibers that make up the TLF are continuous with the muscles and flat tendons from which it is formed, connecting different muscles from different parts of the body. The myofasciae of the trunk are organized in three cylindrical layers—superficial, middle, and deep—and the TLF fibers reflect the same organization. For example, the latissimus dorsi, gluteus maximus, and external obliques are all continuous with the superficial fibers of the TLF. The internal obliques and serratus posterior inferior are continuous with the middle layer of the TLF. And the transversus abdominus, erector spinae, and multifidus muscles are continuous with the deep layer of the TLF. This organization means when the muscles contract, they create forces that transmit through the low-back fascia from different directions and at different depths all day, every day.
Jelly Sandwiches
Let’s zoom in on the TLF microscopic anatomy using a familiar but rather unexpected comparison: a jelly sandwich (Image 2). That’s right, we can understand more about what’s going on between the flat tendons from all these muscles by thinking about sandwiches.
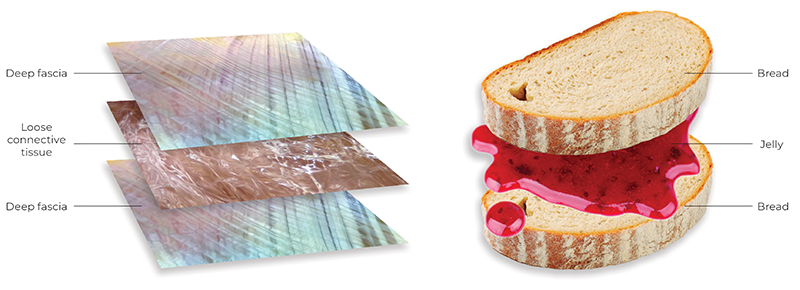
To accommodate the forces that move through the TLF, a different type of tissue is found between the layers—loose connective tissue (Image 3). In our sandwich analogy, the flat tendons are the bread and the loose connective tissue is the jelly. But instead of grapes or strawberries, the low-back “jelly” is made of a lot of water, a few fibers, and hyaluronan (HA). You may have seen hyaluronic acid listed as an ingredient in your face cream—it’s the same stuff. The reason it’s in your face cream is because HA loves water and holds moisture. And who doesn’t want a little moisture on their skin? The scientific term for a substance having a special affinity for water is hydrophilic, which comes from Greek for “water loving.” The HA in loose connective tissue grabs all the available water it can and creates a gel that acts as a slippery lubricant.

Nestled between each fibrous layer of tough, collagen-rich fascia—the bread in our sandwich analogy—is a thin layer of loose connective tissue rich in HA—the jelly. If everything is going according to plan, the HA helps the fibrous flat tendons glide and slide across each other as we bend, twist, and move around, allowing for all those forces to transmit through the TLF hub. When things get a little sticky, however, the jelly can act more like peanut butter, causing movement to be restricted. This happens when the viscosity of the HA increases and additional bonds form, which can be caused by the usual suspects of lack of use, overuse, or misuse. But why does it matter if your loose connective tissue is more like jelly or peanut butter?
Tough but Full of Feelings
TLF is tough, pulled in every direction, but it also has a lot of feelings. How do we know? Researchers have been looking into it and surprisingly discovered that the TLF has a lot of feelings. By staining the TLF with a particular dye under microscopy, it is evident that sensory nerves don’t just pass through the TLF, many end there, picking up information about pressure, stretch, vibration, proprioception, and, you guessed it, nociception. We like to think of nociceptors as the “uh-oh” nerve ending; they signal to the brain that something isn’t right, then you feel pain.
If fascia can feel, and the layers in the TLF are supposed to move in relation to each other, what happens when they don’t? This question made researchers curious too. Research using ultrasound imaging has revealed that the glide between the layers—a.k.a. the jelly side—is reduced in people with low-back pain compared to those without pain. This suggests a correlation between pain and lack of glide. What is interesting is the possibility that the problem may not lie within the tissues of the low back as much as in their relationship to each other. But can the slipperiness of hyaluronan be altered? Yes, and
quite easily.
Thoracolumbar Fascia and Massage
One of the simplest ways to reduce HA viscosity is through heat and mechanical strain. Put another way, the jelly thins out when it is stirred. Enter, you, the massage therapist! Whether you knew it or not, you’ve been “stirring the jelly” in your client’s low-back “sandwiches” all along. When working with the low back, you’re not just addressing individual tissues, you’re also helping all the layers of that sandwich move better together.
Certainly, there are a lot of causes for low-back pain, but when it comes to the nonspecific kind, once everything else has been ruled out, your hands-on work just might be the perfect solution.
Note
1. World Health Organization, “Low Back Pain,” June 19, 2023, https://who.int/news-room/fact-sheets/detail/low-back-pain.
Resources
Balagué, F. et al. “Non-Specific Low Back Pain.” The Lancet 379, no. 9814 (February 4, 2021): 482–91. https://pubmed.ncbi.nlm.nih.gov/21982256.
Fede, C. et al. “Evidence of a New Hidden Neural Network into Deep Fasciae.” Scientific Reports 11, no. 12623 (June 16, 2021). https://nature.com/articles/s41598-021-92194-z.
Langevin, H. M. et al. “Reduced Thoracolumbar Fascia Shear Strain in Human Chronic Low Back Pain.” BMC Musculoskeletal Disorders 12, no. 203 (September 19, 2011). https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-12-203.
Pratt, R. L. “Hyaluronan and the Fascial Frontier.” International Journal of Molecular Sciences 22, no. 13 (June 25, 2021): 6845. https://doi.org/10.3390/ijms22136845.
Schleip, R. et al. “Fascia as an Organ of Communication” in Fascia: The Tensional Network of the Human Body, 2nd ed. Churchill Livingstone Elsevier, 2021.
Stecco, C. Functional Atlas of the Human Fascial System, 1st ed. Churchill Livingstone Elsevier, 2015.
van Dieën, J. H. et al. “Non-Specific Low Back Pain.” The Lancet 379, no. 9829 (May 19, 2012): 1874. https://thelancet.com/article/S0140-6736(12)60803-4/fulltext.








