When we think of joints in the human body that are either important toward proper function and/or often involved in dysfunction, there are a number that might come to mind: the shoulder, hip, or knee; or perhaps the saddle joint of the thumb, disc joints of the spine, or the sacroiliac joint. But there is one joint that is often overlooked and rarely placed on this list, despite the fact it should be—the metatarsophalangeal (MTP) joint of the big toe (Image 1).

MTP Joint
The MTP joint of the big toe is between the first metatarsal and the proximal phalanx. It is a biaxial joint that allows movement in the sagittal and frontal planes (Image 2).


Of these motions, sagittal-plane extension is critically important toward functional movement of the lower extremity. We usually think of standard/open-chain joint actions wherein the distal body part moves relative to the proximal one. Looking at the big toe’s MTP joint, this would be movement of the proximal phalanx relative to the first metatarsal, as shown in Image 2. However, extension of the proximal phalanx at the MTP joint is not very functional in life. After all, how often do we need to lift our big toe up into the air? Instead, the reverse action/closed-chain action of this joint is what is important (see “A Deeper Dive—Open-Chain and Closed-Chain Joint Actions” below).
Closed-Chain MTP Joint Extension
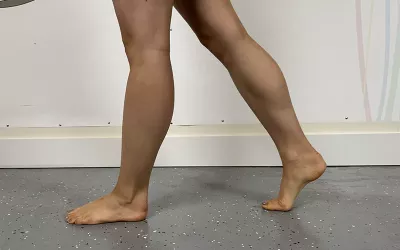
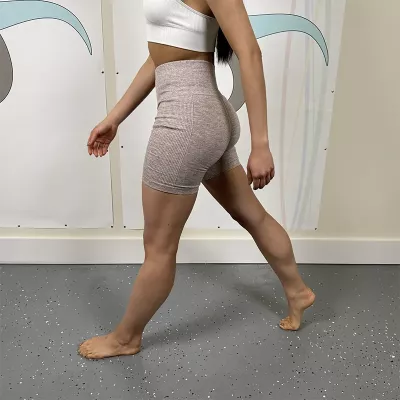
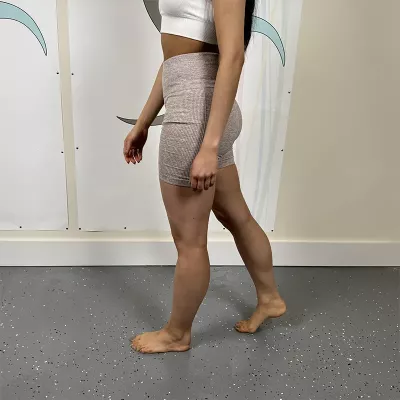
Closed-chain extension of the MTP joint occurs when the proximal phalanx is stable on the ground and the first metatarsal moves relative to it. This occurs with each step of the gait cycle (walking) during the phase of movement known as heel-off, wherein the lower extremity in back is lifting off the ground as the opposite-side lower extremity in front is striding forward. Because the rear foot is stable/fixed against the ground and body weight is moving forward, the natural motion as the heel lifts off the ground is for the metatarsals to move into extension toward the proximal phalanges instead of the phalanges moving toward the metatarsals (Image 3).
And because the foot naturally moves into supination at the subtalar joint during heel-off, much of this motion occurs more medially in the foot at the big toe instead of the other toes. In effect, the foot pivots at the big toe’s MTP joint. Therefore, the principal functional joint motion at heel-off is closed-chain extension of the first metatarsal relative to the proximal phalanx at the MTP joint (Image 4).

Kinematic Consequence: Stride Length
The reason MTP joint extension is such a critical movement, and therefore the MTP joint of the big toe is such an important joint, is that if big toe MTP extension is limited, then stride length during the gait cycle is decreased. Looking at heel-off during the gait cycle, for the limb in back to allow a normal stride length, a number of joint actions must occur—hip joint extension, knee joint extension, ankle joint plantar flexion, and big toe MTP joint extension (Image 5A). Motions of the lower extremity are very interdependent. If any one of these motions is limited, then all these motions will be limited, hence stride length decreased (Image 5B).
And if stride length decreases on one side, then for symmetry of how we walk, it must decrease on the other side too. Looking at the other side, as the limb in back is in heel-off (then toe-off), the limb in front is in heel-strike and then foot-flat. At heel-strike and foot-flat, the limb in front has the following motions: hip joint flexion, knee joint extension, and ankle joint dorsiflexion (at heel-strike).
Decreased Stride Length
Limited MTP extension in one foot decreases stride length on both sides. Let’s take a closer look at the consequences of this at the hip joint. Let’s begin with the forward-striding lower extremity. The forward-striding limb involves flexion at the hip joint. However, if the stride length is decreased, then decreased hip flexion results in less stretch of the hip extensors, especially the hamstrings (Image 5B). And if we do not stretch the hamstrings as much, they will likely become tighter.
Tight Hamstrings
What is the consequence of tight hamstrings? Tight hamstrings can cause excessive posterior tilt of the pelvis, with concomitant hypolordosis of the lumbar spine. Lumbar hypolordosis is, by definition, decreased extension; in other words, it is increased flexion. Increased lumbar flexion shifts weight-bearing from the more posterior facet joints onto the more anterior disc joints. This can lead to disc pathology, including bulging and herniated discs. Also, changes in the posture of the lumbar spine will result in postural compensations all the way up the spine.
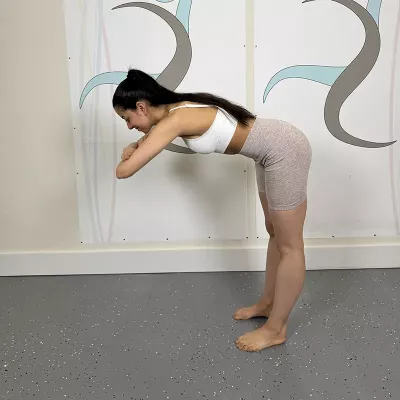
Furthermore, tight hamstrings make tight backs. When a person stretches forward, for example to pick up something from the ground, if the hamstrings are tight, it increases the demand for the low-back extensor musculature (e.g., paraspinal erector spinae) to stretch/overstretch, often causing a muscle spindle/stretch reflex, thereby causing tight low-back muscles, likely causing pain. Chronic tightness of the low-back muscles then results in increased compression of the disc joints, further increasing the possible likelihood of pathologic disc disease (bulging/herniation), as well as osteoarthrotic bone spurs, which could then increase the likelihood of nerve compression and sciatica. Again, all this can follow from a hypomobile MTP joint of the big toe!
Tight Hip Flexors
Of perhaps even greater importance, let’s look at the effect of decreased stride length on the lower extremity in back. When the limb in back has limited stride length, there is less hip joint extension; and hip joint extension is critical for stretching the hip flexors. Therefore, due to a lack of stretching of the hip flexors, there is a direct correlation between decreased MTP joint extension and tight hip flexors. This then has continuing consequences up the kinematic chain. Tight hip flexors, or what are called locked-short hip flexors, when standing, play out their tightness with the reverse/closed-chain joint action of anterior tilt of the pelvis at the hip joint (Image 6). This results in the postural distortion pattern of increased pelvic anterior tilt, which is the fundamental cause of lower-crossed syndrome.

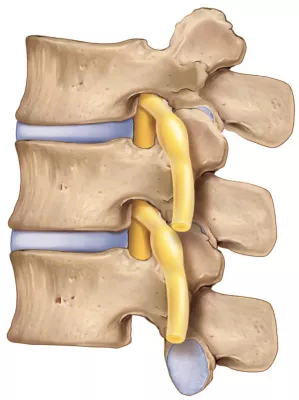
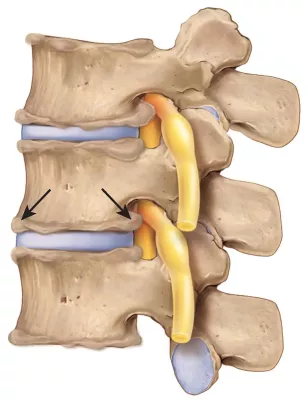
Lower-Crossed and Upper-Crossed Syndromes
Lower-crossed syndrome is characterized by increased anterior pelvic tilt, causing hyperlordosis of the lumbar spine, with increased weight-bearing and jamming of the lumbar facets, which can cause facet syndrome, resulting in low-back pain. Chronic facet syndrome increases the likelihood of osteoarthrotic bone spurs. If these bone spurs protrude into the intervertebral foramen (IVF), this could cause compression of the nerve root as it passes through the IVF (called lateral canal stenosis), which in the low back could result in sciatica (Image 7).
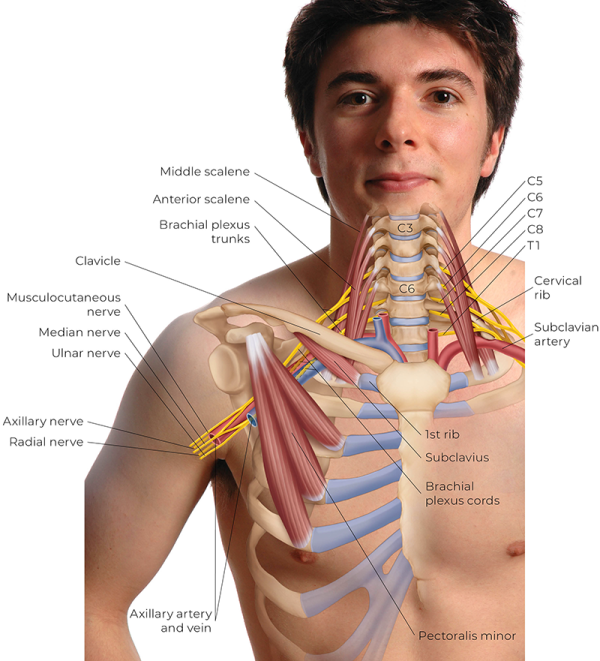
Continuing up the kinematic chain, lumbar spine hyperlordosis will precipitate hyperkyphosis of the thoracic spine, which then follows with hypolordosis of the lower cervical spine and hyperextension of the head at the atlanto-occipital joint, with forward-head posture. This upper body postural distortion pattern is known as upper-crossed syndrome. This then increases the tension of the cervicocranial extensor musculature (e.g., upper trapezius, semispinalis capitis, levator scapulae), resulting in a tight and painful neck and an increased likelihood of tension headaches. We could even see that the cervical hypolordotic curve could cause locked-short lower-to-middle cervical spine flexors, resulting in tight sternocleidomastoids, scalenes, and hyoid muscles. Tight scalenes can increase the chance of anterior scalene syndrome, a type of thoracic outlet syndrome. Tight hyoids would increase stress on the temporomandibular joints (TMJs), contributing to the possibility of developing TMJ dysfunction.
Another consequence of thoracic hyperkyphosis is rounded/protracted shoulder girdles and increased medial rotation of the arms at the glenohumeral joints. The increased glenohumeral medial rotation then increases the likelihood of shoulder impingement syndrome due to the approximation of the greater tubercle of the humerus with the acromion process above during abduction motions of the arm. And shoulder impingement syndrome usually results in subacromial bursitis as well as supraspinatus rotator cuff degeneration and possible tearing, which then increases the risk of frozen shoulder.
Returning to the thoracic hyperkyphosis and protracted shoulder girdle posture of upper-crossed syndrome, the risk of all three forms of thoracic outlet syndrome (anterior scalene, costoclavicular, and pectoralis minor syndromes) then dramatically increases (Image 8).
Further, thoracic hyperkyphosis is, by definition, increased flexion (kyphosis is a curve of flexion), which likely leads to decreased thoracic spine extension range of motion. Decreased thoracic extension then places a greater load on the lumbar spine to extend when spinal extension is needed, further increasing the lumbar lordosis and playing into the vicious cycle begun by the excessive anterior pelvic tilt.
Thus, the lowly MTP joint of the big toe, if restricted in extension, can have far-reaching effects in the body, affecting the hip joints, TMJs, glenohumeral joints, shoulder girdles, thoracic outlet syndromes, headaches, and lumbar, thoracic, and cervical spine. Fairly incredible! Of course, not every one of these conditions will necessarily follow, but the likelihood of these conditions increases with decreased MTP extension.
Causes of Decreased Extension at the MTP Joint
This then begs the question: Why might the MTP joint have decreased extension? One major reason is high-heeled shoes. Another is overpronation of the foot.
High-Heeled Shoes
When barefoot, the normal weight distribution through the foot is approximately 50 percent through the calcaneus and 50 percent through the metatarsal heads. However, when the heel is lifted, the proportion of weight-bearing through the metatarsal heads increases, thereby increasing physical stress into the MTP joints (Image 9). This can result in irritation and inflammation and the likely development of osteoarthrosis at the MTP joints and especially at the first MTP joint given that most of the force of heel-off (and toe-off) occurs through the big toe’s MTP joint.

Further, given that most people wear shoes that have a narrow toe box, the big toe is pushed in the lateral direction, resulting in hallux valgus of the big toe with its characteristic formation of a bunion; all this leads to further physical stress to the MTP joint. Although women’s high heels are the worst culprit, men’s shoes also often have a raised heel and a narrow toe box. If we wind all this back, we see that wearing high heels might likely result in MTP joint dysfunction and, therefore, every one of the conditions we have named in this article.
Overpronation
Another major cause of dysfunctional movement at the MTP joint of the big toe is overpronation. Pronation is a natural and healthy motion of the foot that involves eversion, abduction, and dorsiflexion at the subtalar joint. However, if pronation is excessive, it can have strong biomechanical consequences on the big toe and, indeed, the rest of the body. An easy way to visualize overpronation is to picture collapsing of the arch structure of the foot. The first obvious visual sign of this is to see the medial longitudinal arch dropping (Image 10).

But another aspect of overpronation is the foot abducting outward (Image 11). The consequence of this is that as body weight shifts through the foot during the gait cycle, instead of distributing weight somewhat evenly over all the toes, the force of body weight is placed excessively over the big toe, which given the angle of force, then splays the big toe laterally outward, a condition known as hallux valgus, along with the characteristic bunion that accompanies this condition. All this results in increased stress and dysfunction at the MTP joint of the big toe, which in time results in decreased extension. The causes of overpronation are many and, therefore, beyond the purview of this article. What is important to note here is that the therapist needs to address not only the direct hypomobility of the MTP joint but also the underlying causes.

Role of the Massage Therapist
What role can massage and manual therapists play when working with clients who experience decreased MTP joint extension of the big toe? Let’s begin by assessing the extension range of motion of the big toe’s MTP joint. There should be approximately 80 degrees from anatomic position. If we find that extension is decreased, then we can begin by massaging and warming up the tissues of the foot and (lower) leg, with special focus on the flexor muscles of the toes, both extrinsic from the leg and intrinsic wholly located within the foot. After warming the tissue with massage (and perhaps heat), we can begin stretching the MTP joint into extension (Image 12).

If it is within the scope of our license and training, we can also perform slow-oscillation Grade IV joint mobilization; dorsal glide is especially important (Image 13). Further, given all the possible consequences of this condition, it would be prudent to assess for, and treat if found, any of the consequences up the kinematic chain.


Another major role is to counsel the client regarding healthy footwear. If we find that the client is wearing higher-heeled shoes, then recommending that they gradually transition toward a lower heel is of paramount importance. It is also important to assess for overpronation, and if found, treat this appropriately. This could be a passive treatment, such as recommending orthotics to the client, or it could be more active, looking to address the myofascial- and joint-related causes.
In conclusion, when we assess our clients, although the MTP joint of the big toe might seem distant from the locus of pain and discomfort reported by the client, this is a critically important joint to consider as part of the possible kinematics of the client’s condition. Therefore, I recommend assessing MTP joint extension as a part of our physical exam with all new clients. And, if decreased extension range of motion is found, perform the appropriate treatment.
A Deeper Dive—Open-Chain and Closed-Chain Joint Actions
When learning muscles, it's typical to learn the muscle’s joint actions wherein the distal attachment/body part (usually termed the insertion) moves relative to the proximal attachment/body part (usually termed the origin). This type of joint action can be described as the open-chain action. Let’s look at the ankle joint of the lower extremity as an example. The lower extremity can be described as having four elements in its kinematic chain: the pelvis, thigh, (lower) leg, and foot. When the foot is in the air, and therefore free to move, we describe the lower extremity as being open-chain. And when we are in open-chain, because the foot is lighter than the leg, movement at the ankle joint would usually result in movement of the foot relative to the leg.
However, if the foot is in a closed-chain position against a stable surface, hence the distal link in the chain of kinematic elements is closed, then when movement occurs at the ankle joint, because the foot cannot easily move, the leg moves relative to the foot. For example, instead of open-chain dorsiflexion of the foot relative to the leg at the ankle joint (Image A), we can have closed-chain dorsiflexion of the leg relative to the foot at the ankle joint (Image B).











