Alarmist alert: The following statements are all true. But the consequences are not always as dire as portrayed here.
Scenario 1
Picture a virus that moves easily from human to human through saliva and respiratory secretions, sexual activity, and contaminated skin-breaking gear like needles or tattoo equipment. It can also be shared indirectly via fomites like toothbrushes or drinking glasses.
This virus can cause infections that are completely silent, but when symptoms are present, they often involve a sore throat, debilitating fatigue, a risk of splenic rupture, dangerous reactions to antibiotics, and a post-viral syndrome with possible life-changing, long-term consequences.
This virus evades the immune system by hiding in its target cells after the infection subsides. From there, it can reactivate to cause repeated, silent outbreaks, during which it can spread to other hosts.
But that’s just the beginning. In addition to causing an acute infection, this virus can also cause pneumonia, pancreatitis, hepatitis, myocarditis, and various inflammations of the central nervous system. And it is one of the few pathogens directly associated with a variety of cancers: Burkitt’s lymphoma, Hodgkin’s and non-Hodgkin’s lymphoma, nasopharyngeal cancer, and others.
And it is everywhere. It is virtually inescapable. We have no strategies to prevent transmission, no vaccine, and no protective measures. Consequently, about 95 percent of adults have it. You, dear reader, almost certainly harbor colonies of this pathogen, even if you have no memory of symptoms or an infection.
Scenario 2
Imagine a disease. It’s been in the medical literature for about 150 years, but has been present for much longer. We don’t know everything about it, but we know a lot, and we’re learning more all the time.
This disease causes scattered patches of damaged tissue and scarring to appear throughout the brain and spinal cord. These lesions interfere with nerve transmission, so both sensation and motor control in the rest of the body are affected.
Symptoms of this disease may vary from one episode to the next, and might include brain fog, fatigue, vision disturbances, painful muscle spasms, weakness, loss of balance, and gastrointestinal dysfunction, among many other possibilities. It is often progressive, and patients may accrue permanent damage to both glial cells and axons in the central nervous system (CNS).
This disease is not necessarily terminal, but it is associated with loss of ambulation and diminished bowel and bladder control, among many other problems. Complications related to lost function shorten the lifespan of people with this condition by an average of 5–10 years.
How Do These Two Scenarios Connect?
We have suspected for a long time that the pathogen in the first scenario, Epstein-Barr virus (EBV), which causes mononucleosis, might have something to do with the disease in the second scenario, multiple sclerosis (MS). But a recent large-scale study points out a much closer connection than we knew—this virus might actually cause MS. This discovery may change future strategies and outlooks for people with either or both of these situations.
Multiple Sclerosis: An Overview
In 1868, a French neurologist named Jean-Martin Charcot, a pioneer in neuroanatomy, described what he labeled la sclérose en plaques. He distinguished what we now call multiple sclerosis from other CNS conditions, especially Parkinson’s disease. Charcot identified three common symptoms of MS—nystagmus, intention tremor, and disrupted speech patterns. This presentation is now called the Charcot triad.
MS affects about 400,000 people in the US, and about 2.1 million people worldwide. It is usually diagnosed in young adults between the ages of 20 and 40. Women are diagnosed about twice as often as men. This disease is most common among people who spend the first part of their lives at latitudes far from the equator, which has led to some speculation about contributing factors and treatment options.
MS Pathophysiology
To talk about MS, we must briefly review the role of myelin. Myelin is an insulating layer of proteins and fats that wraps around neuron fibers. Myelin helps speed nerve transmission and insulate electrical impulses within tightly packed bundles of neurons. In the CNS, it is light-colored, so myelin-wrapped brain and spinal cord tissue is referred to as white matter.
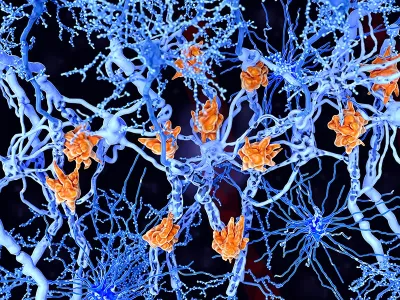
MS involves an attack with elements of both innate and adaptive immunity turned against myelin sheaths within the CNS. When myelin breaks down, a few bad things happen: Function is lost at the affected neurons, so impulses cannot carry through to their destinations; local inflammation can damage tissues all around the affected area; and scar tissue plaques develop at the sites of attack. Ultimately, the damage may penetrate beyond the myelin-producing cells to affect the axons.
MS has several different presentations, but the most common form, relapse/remitting MS, involves clear cycles of flare and remission. Sometimes patients can begin with one type, and then go on to develop a different form of the disease. For more on types of MS and what it’s like to live with it, see the video that accompanies this article.
Signs and Symptoms of MS
MS is sometimes called “the great imitator” because during flares it can look like a myriad of other diseases or conditions. Symptoms may become severe during episodes of flare, and then subside during remission. In early stages, remission may bring about a full restoration of function. But as the disease progresses, some loss of function may be permanent.
Signs and symptoms of MS are sometimes discussed as primary issues related directly to the destruction of myelin, and secondary problems that are complications of the primary ones.
Primary issues include debilitating fatigue, weakness, numbness, paresthesia, trouble swallowing, tremors, vision problems, loss of balance, pain, paralysis, and bladder and bowel problems. All of these are brought about by myelin damage to the associated motor and sensory neurons.
Secondary issues can include pressure sores related to paralysis, urinary tract infections from bladder weakness, muscle deconditioning leading to atrophy, bone thinning from inactivity and steroid treatments, injuries from falls with a risk of fracture, and pneumonia related to inactivity and/or aspiration due to an impaired swallow reflex.
Ultimately, a person with MS may become impaired enough to require assistive equipment in the form of a walker or wheelchair. They may not be able to drive or live independently. The strain of dealing with a chronic long-term illness can also take a toll on relationships and mental health. Depression is a frequent outcome of MS, and it can make treating MS more difficult.
Theories About MS: Genetics and Environmental Exposures
Genetic mutations that contribute to the risk of developing MS have been identified, and studies done through the International MS Genetics Consortium continue to explore this aspect of the disease. But family history of MS appears to be a relatively minor risk factor.
The development of MS is also related to two important types of environmental exposures: sunlight and pathogens.
Sunlight, Latitude, and Vitamin D
We have known for decades that MS is more common in people who live far away from the equator, but the exact processes that lead to this outcome aren’t completely clear. It has been established that the first 12 years of life are a determining factor; children who are born and spend their childhood in the far north or the far south have a greater chance of developing MS than those born closer to the equator.
However, children born in northern latitudes can benefit from sun exposure: 30 minutes a day in sunshine (with appropriate sunscreen) appears to reduce the risk of developing MS later in life. This may be especially important for children who have a close relative with MS.
Another connection between sunlight exposure and MS lies in the production of vitamin D. We produce vitamin D when we are exposed to the sun. People who have MS often have low serum levels of vitamin D and have fewer flares when they supplement this vitamin. The action of vitamin D as a guard against MS flares isn’t fully understood, but it may play a role in immune system function.

EBV
Many people are familiar with EBV because this is the virus that causes mononucleosis (mono), an infection that begins in the epithelial tissue of the throat and salivary glands, and then moves into the lymph nodes. Mono elicits an aggressive immune system response, leading to fever, sore throat, enlarged and painful lymph nodes (including the spleen), and debilitating fatigue.
As we discussed at the beginning of this column, an EBV infection can be subtle and uneventful, but for some people it can lead to much more serious consequences, including pneumonia, cardiomyopathy, CNS inflammation, certain kinds of cancer, and much more.
EBV is a member of the Herpesviridae family, along with herpes simplex, varicella zoster (the virus that causes chicken pox and shingles), cytomegalovirus, and others. All members of the Herpesviridae family have one feature in common: they are never fully eradicated from the body. Instead, a viral colony goes dormant inside some target cells. The target cells for EBV are memory B-cells.
Scientists have long suspected that MS might be related to a history of pathogenic exposures. This is common in autoimmune disorders: The immune system encounters an invader, and then later mistakes some part of the body as that invader. But interest in EBV as a precipitator for MS recently took a giant leap forward with the results of one of the biggest studies in history.
When an American enrolls in the military, they commit to undergo a blood test for HIV every two years for all the years they are in service. Blood samples from these tests may also be examined for other pathogens or disease markers.
Researchers tracked blood samples from more than 10 million US military personnel over a span of 10 years. (You read that correctly.) The team made a variety of findings, but the most striking one was the strong correlation between EBV exposure and the risk of developing MS.
The researchers were able to use blood tests to identify when subjects were exposed to EBV, which often happens in young adulthood. They found that the risk of developing MS increased 32-fold after an EBV infection—a change that was not seen with exposure to other viruses. The average onset of MS symptoms was about 10 years after EBV exposure, but early markers of the disease were distinguishable before symptoms developed.
The research team also found that coinfection with cytomegalovirus, a closely related pathogen, seems to impart some (but not full) protection from MS. Finally, among the subjects who were not exposed to EBV, none developed MS.
It is important to bear in mind that having a history of mono or EBV exposure does not mean a person will inevitably develop MS—otherwise we’d all be in treatment! But there does seem to be a causative relationship between EBV exposure and MS for people who have other risk factors for the disease.
What does this mean for the future understanding of MS? This discovery could lead to a few different possibilities. Our experiences with COVID and flu have taught us the usefulness of antiviral medications. Because EBV exposure doesn’t just precipitate MS, but appears to have an ongoing influence on the development of this disease, it is possible that antiviral medications that target EBV might also change the course of MS in a patient who already has it.
In addition, an anti-EBV vaccine is currently in early-stage clinical trials in humans. If this bears fruit, then one day we will have a way to prevent mono, EBV-related cancers, MS, and much more.
Implications for Massage Therapy?
Does the discovery that EBV might be a causative factor in the development of MS change anything about the best role for massage therapy in this context? Probably not—at least not yet. But MS affects a lot of people, and EBV is extremely common, so as health-care providers we should have this on our radar.
Hygienic practices to prevent new EBV infection are probably pointless, since most adults already have it. When we get to the point of using antivirals to treat this situation, or vaccines to prevent EBV, then we will have to make decisions based on whatever side effects these interventions may cause. Until then, we can fall back on our current understanding of the best ways massage therapy can help people with MS. Some people with MS experience weakness or spasm in the extremities. Slow, comfortable, and predictable massage can be used to minimize this.
Massage that is too deep or too fast can sometimes stimulate painful and uncontrolled muscle contractions, even for clients who are in remission. Areas of numbness or changed sensation call for special caution, since clients may not be able to identify uncomfortable pressure. Sudden changes in stimuli, including pressure, temperature, and other variables, appear to be difficult for many people with MS to process, so using ice, heat packs, or even table warmers may not be practical for clients with this condition.
We have research findings in favor of massage therapy for fatigue, pain, and constipation related to MS. The data on massage therapy as a strategy to preserve or improve muscle function is less clear. But people with MS are enthusiastic consumers of our work, and that means we have an obligation to be well-informed about their needs and requirements.
And, given these new findings, the day may come when EBV-related illnesses like MS will be remnants of the past, and articles like this will become historical artifacts. And won’t that be an amazing day?
Resources
Bjornevik, K. et al. “Longitudinal Analysis Reveals High Prevalence of Epstein-Barr Virus Associated with Multiple Sclerosis.” Science 375, no. 6578 (2022): 296–301. https://doi.org/10.1126/science.abj8222.
Centers for Disease Control and Prevention. “About Epstein-Barr Virus (EBV).” Last reviewed September 28, 2020. www.cdc.gov/epstein-barr/about-ebv.html.
Centers for Disease Control and Prevention. “Epstein-Barr and Mononucleosis For Healthcare Providers.” Last reviewed September 28, 2020. www.cdc.gov/epstein-barr/hcp.html.
Doctrow, Brian. National Institutes of Health. “Study Suggests Epstein-Barr Virus May Cause Multiple Sclerosis.” February 1, 2022. www.nih.gov/news-events/nih-research-matters/study-suggests-epstein-barr-virus-may-cause-multiple-sclerosis.
Frost-Hunt, A. “Effects of Massage Therapy on Multiple Sclerosis: A Case Report.” International Journal of Therapeutic Massage & Bodywork. 13, no. 4 (2020): 35–41.
George, Judy. MedPage Today. “Sun Exposure May Protect Against Pediatric-Onset MS.” December 10, 2021. www.medpagetoday.com/neurology/multiplesclerosis/96142.
Harvard T. H. Chan School of Public Health. “Epstein-Barr Virus May Be Leading Cause of Multiple Sclerosis.” January 13, 2022. www.hsph.harvard.edu/news/press-releases/epstein-barr-virus-may-be-leading-cause-of-multiple-sclerosis.
Houen, G. and N. H. Trier. “Epstein-Barr Virus and Systemic Autoimmune Diseases.” Frontiers in Immunology 11 (January 7, 2021). https://doi.org/10.3389/fimmu.2020.587380.
Huang, W. J., W. W. Chen, and X. Zhang. “Multiple Sclerosis: Pathology, Diagnosis and Treatments.” Experimental and Therapeutic Medicine, 13, no. 6 (2017): 3,163–66. http://doi.org/10.3892/etm.2017.4410.
Johns Hopkins Medicine n.d. “Multiple Sclerosis (MS).” www.hopkinsmedicine.org/health/conditions-and-diseases/multiple-sclerosis-ms.
Luzzio, Christopher. Medscape. “Multiple Sclerosis.” January 3, 2022. https://emedicine.medscape.com/article/1146199-overview.
MS International Federation. “Researchers Strengthen the Link Between Epstein-Barr Virus (EBV) and the Risk of Developing MS.” March 29, 2022. www.msif.org/news/2022/01/21/researchers-strengthen-the-link-between-epstein-barr-virus-ebv-and-the-risk-of-developing-ms.
National Institutes of Health. “Epstein-Barr Virus and Autoimmune Diseases.” April 24, 2018. www.nih.gov/news-events/nih-research-matters/epstein-barr-virus-autoimmune-diseases.
National Institute of Allergy and Infectious Diseases. “NIH Launches Clinical Trial of Epstein-Barr Virus Vaccine.” May 6, 2022. www.niaid.nih.gov/news-events/nih-launches-clinical-trial-epstein-barr-virus-vaccine.
National Institute of Allergy and Infectious Diseases. “NIH Researchers Make Progress Toward Epstein-Barr Virus Vaccine.” April 9, 2019. www.niaid.nih.gov/news-events/nih-researchers-make-progress-toward-epstein-barr-virus-vaccine.
National Multiple Sclerosis Society. “Massage and Bodywork.” Accessed July 2022. www.nationalmssociety.org/Treating-MS/Complementary-Alternative-Medicines/Massage-and-Body-Work.
Negahban, H., S. Rezaie, and S. Goharpey. “Massage Therapy and Exercise Therapy in Patients with Multiple Sclerosis: A Randomized Controlled Pilot Study.” Clinical Rehabilitation. (2013): 1,126–36. https://doi.org/10.1177/0269215513491586.
Orrell, R.W. “Multiple Sclerosis: The History of a Disease.” Journal of the Royal Society of Medicine 98, no. 6 (2005): 289.
Pietrangelo, Ann. “Can Massage Help With MS Symptoms?” Updated July 29, 2018. www.healthline.com/health/ms-massage.
Sabel, C.E. et al. “The Latitude Gradient for Multiple Sclerosis Prevalence is Established in the Early Life Course.” Brain 144, no. 7 (2021): 2,038–46. http://doi.org/10.1093/brain/awab104.
Salarvand, S. et al. “Effectiveness of Massage Therapy on Fatigue and Pain in Patients With Multiple Sclerosis: A Systematic Review and Meta-Analysis.” Multiple Sclerosis Journal—Experimental, Translational and Clinical 7, no. 2 (2021). https://doi.org/10.1177/20552173211022779.
Science Daily. “Epstein-Barr Virus May Be Leading Cause of Multiple Sclerosis.” January 13, 2022. www.sciencedaily.com/releases/2022/01/220113151342.htm.
Simpson, S. et al. “Latitude Continues to be Significantly Associated With the Prevalence of Multiple Sclerosis: An Updated Meta-Analysis.” Journal of Neurology, Neurosurgery, and Psychiatry. 90, no. 11 (2019): 1,193–1,200. https://doi.org/10.1136/jnnp-2018-320189.
Wood, Heather. “Latitude and Vitamin D Influence Disease Course in Multiple Sclerosis.” Nature Reviews Neurology 13, no. 3 (2017). http://doi.org/10.1038/nrneurol.2016.181.








