As massage therapists, we see our clients’ scars all the time. If the scar is new, we tend to think locally—we assess the scar’s texture, appearance, symptomology, size, direction, skin restriction, scar type, and phase of healing.¹ But what if there is more to it? What if there is more happening under the skin than meets the eye?

While it’s always good to assess and treat a scar locally, depending on its depth and size, a scar can have widespread implications leading to chronic pain, potential complications in future injuries, restricted range of motion, and, ultimately, an impact on quality of life. With the advancement of fascial research, we are only beginning to understand the extent of the disruption scars create in the ecosystem within the fascial network.
In postoperative cases, scar tissue has one of the most variable outcomes.² Rehabilitative therapists understand that scar tissue can pose an issue; however, it’s not well understood how.³ Scar tissue is the result of a disruption in the continuity of the connective tissue that can impact a multitude of systems in the body, including the lymph, fascial, vascular, skeletal, and neural systems.4 To say “it’s all connected” is no longer enough.
Therapists endeavor to “loosen” the scar, but the bigger picture is that we are helping to reintegrate scars into the fascial matrix. This is the benefit of the postsurgical work we do.
With modern technology, we understand these systems are undoubtedly connected, interconnected, and even interdependent. When a therapist applies a broader perspective of scar tissue in the context of this interconnection (such as the principles of biotensegrity to the fascial system), we see that a scar is not just a scar but a tear in our biological spiderweb that the body urgently seeks to bind and repair to regain its tensile function.5 Scars are not just thickened tissue; they are a testament to self-preservation. How we approach scars as manual therapists can make all the difference in our clients’ quality of life. Recent research suggests there may be a “map” to help us in that process.
Impacts and Interventions
Scars may arise from various causes, including falls, accidents, and often from surgical procedures designed to alleviate pain, restore function, or save lives.

Common surgical interventions our clients might experience include:
- Appendectomy
- Biopsies or lumpectomy
- Cardiac procedures
- Cesarean section
- Hernia repairs
- Hysterectomy
- Joint replacements
- Mastectomy
- Spinal surgeries
- Tonsillectomy6
The postoperative phase of a surgical event marks the beginning of a patient’s recovery process. It’s also a time when complications such as infection, thrombosis, significant pain, and swelling can prolong recovery. Massage is not currently indicated for direct treatment of healing tissue. However, in the immediate aftermath, we have an excellent opportunity to indirectly help our client’s healing by calming their nervous system (which can also help modulate their inflammation) and apply lymphatic therapy for their swelling.7 Our ability to assist clients in their recovery is improved with early intervention and frequency of care.
The Healing Journey
The acute phase, the initial time following injury or surgery, encompasses hemostasis and inflammation—the body’s mechanisms for halting blood loss and mobilizing immune responses. It’s the body’s all-hands-on-deck alert that ushers in the healing cascade.
Cytokines (cell proteins) facilitate communication throughout the system, prompting reinforcement at the wound site. The subsequent proliferative, or subacute, phase involves tissue and vascular reconstruction (granulation) and rebuilding of epithelial tissue (re-epithelialization). Fibroblasts migrate to the damaged area, morph into myofibroblasts (fibroblasts with muscle contractile function), and contribute to wound closure, while cellular debridement removes necrotic tissue.
This process may last weeks to months, depending on wound characteristics and healing efficacy. As noted, practitioners should ensure adequate tissue healing before manual therapy. Typically, this is around 6–8 weeks for uncomplicated scars. A good rule of thumb is if the client is no longer using a bandage, it generally indicates potential readiness for manual therapy. Still, it’s critical you use your best judgment. It’s best to start with light work for a short time to see how the client feels and responds.
The final chronic or remodeling phase in wound healing, potentially spanning years, features collagen maturation and reorganization, during which tissue adapts at the cellular level.8
The Living Web—Fascia’s Role in Scar Tissue
Understanding the complexity of scar tissue starts with understanding the bigger picture. When working with clients, consider that the seemingly inert scar under your hands has more going on than meets the eye. That’s what the fascial system has been teaching us the past few decades. We now recognize the fascial system is not just an inert filler but an incredible three-dimensional, body-wide ecosystem of interconnectedness across multiple systems of communication and functionality. And that interconnectedness applies to scars too.
The fascial system comprises a membranous network that adapts, glides, and separates every anatomical structure.9 This complex, multidirectional network facilitates efficient mechanotransduction (cell communication), reciprocal communication (afferent and efferent signals), nutrient distribution (lymph, vascular, etc.), and the mechanical demands of movement (force transfer).
The concept of tensegrity was introduced by Buckminster Fuller and further developed into biotensegrity by Dr. Steven Levin. This concept explains how bodily integrity arises from the dynamic interplay between tension and compression, governed by principles of energy efficiency and structural stability. There are three principles that help to enact this theory: (1) forces take the shortest path, typically a straight line, (2) structures are closely packed in the most stable structure possible, and (3) the body’s tissue and structures seek the most efficient usage of energy.10
Dr. Robert Schleip and many other researchers have discovered that the fascial system has an abundance of innervation. With over 250 million nerve endings, the fascial system is one of our richest sensory organs. Eighty percent of our sensory information comes from polymodal free nerve endings sensitive to all pressure, temperature, tactile, chemical, proprioception, equilibrium, and pain sensory information. The other 20 percent is comprised of nerve endings such as Ruffini, Pacinian, and Golgi tendons and muscle spindles. All this to say, our body is sending somatosensory signals and receiving motor signals from the brain on a constant basis.
Research indicates the body, and thus our fascia, compensates after injury by redistributing tension to maintain balance. Evidence also suggests that longstanding scars may disrupt the range of motion, gait, and posture and predispose individuals to future complications.11 Therapists endeavor to “loosen” the scar, but the bigger picture is that we are helping to reintegrate scars into the fascial matrix, facilitating normal force distribution and fluid dynamics.12 This is the benefit of the postsurgical work we do.
New Information Leads to More Questions
The fascial system is still largely uncharted territory; therefore, we need to keep exploring. If the fascial system is three-dimensional, the questions then arise: Is scar tissue three-dimensional too? If the body functions based on biotensegral principles, then does scar tissue also function with the same principles? And if so, what does that look like?
My 15 years of experience in the injury treatment/rehabilitation arena and my documentation of numerous clinical observations have informed my emerging theories on predictable scar-related fascial restrictions. This work was born from the struggles in working with some clients over the years who, because of their pain sensitivity, could not handle the deep tissue techniques I had been trained in. These observations would turn out to be the foundation for my research, “A Hypothesized Bio-Tensegral Model for Scar Tissue, Observed in Anterior Cruciate Ligament Reconstruction Surgeries: A Case Report Series” (see below), which was presented at the 2022 Fascial Research Congress and the 2025 International Massage Therapy Research Conference.
Let’s explore some of these early observations that fueled my work, which today has evolved into Omni Scar Therapy—a trauma-informed, evidence-based approach theorizing predictable lines of restriction following tissue injury.
In Image 1, you can see a client’s knee a few years after her anterior cruciate ligament (ACL) reconstruction. The scar is indicated with the green circle. There is a long blue line that runs vertically along the length of the leg and in congruence with the scar. We will call this the “scar line.” These lines are typically the same width as the scar. They can be found far from the scar, such as the nearest joints, and farther.
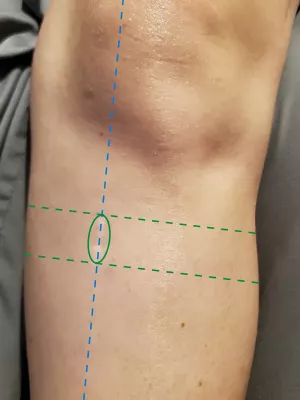
Now find the two green lines in the image that run more horizontally in relation to the scar line—we will call these the “support lines.” They typically span the circumference of the limb. In my findings, there are always two of these at the ends of the scar. The tissue between these two lines tends to be more restricted and guarded. We’ll refer to the combination of these lines as “the pattern.” The patterns appear to pin down and moderately restrict all biological structures and tissue in the direction and circumference of the scar. Because many scars appear as straight lines, the support lines are at either end of the scar as a result. Nuance of the theory is needed when the scar shapes become nonlinear, but this pattern is still present.
When it’s just one scar, it’s easy to mentally apply the pattern. When there are more scars, such as surgeries with multiple incision points, each scar then needs the pattern to be applied to it.
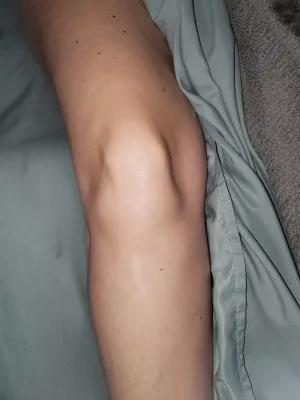
In Image 2, you see pre- and postoperative photos of a client who tore her ACL. The third image indicates the pattern applied to all the small scars. The scar lines can be found as distally as the ankle joint and as proximally as her ilium. The support lines wrap the circumference of her knee, locking in the posterior musculature. With this image, it’s possible to imagine how an entire limb’s range of motion might be limited or impacted by this pattern during the rehabilitation process, which is very common for us to see as therapists.

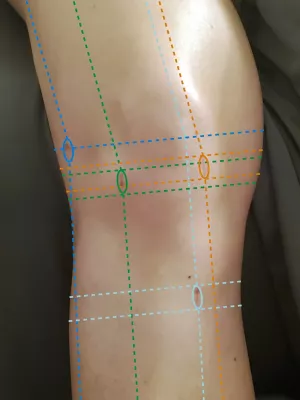
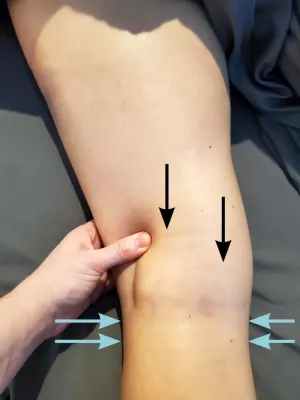
The restrictive patterns can sometimes be seen and verified with palpation. In Image 3, you’ll see a collage of visual observations from my case report series of scar restriction patterns.
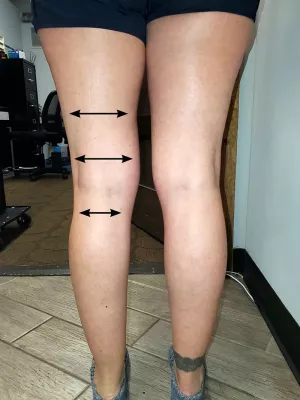



When restriction subsides, range of motion improves. Image 4 shows an active range of motion (AROM) comparison between the first and fifth hands-on sessions. The client spent three years in physical therapy after her reconstructive surgery. She had difficulty with her knee flexion, but after five sessions of applying myofascial release to her scar restriction pattern, she gained 62 percent improved AROM. She was able to return to her active life and ran her first half-marathon since her injury.


Theories on the Restrictive Patterns
What causes these bands of restriction? Here are a few of my theories on why these restrictions exist.
A Secondary Retinacula
Functionally, these bands potentially serve as secondary retinacula, providing real-time biofeedback to the central nervous system and maintaining vigilance over vulnerable regions. Release of such restrictions can restore range of motion after a few sessions without recurrence, provided no further injury occurs.
Re-Tensioning a Pre-Tensioned System
The restrictions potentially assist with immobilization and wound closure, consistent with biotensegrity principles wherein tensile elements facilitate tissue recovery. Earlier, it was mentioned that the fascial system functions within biotensegrity principles. One principle is the idea that the fascial system is pre-tensioned. The epidermis, dermis, and subcutis are parts of this pre-tensioned system. When a wound occurs, the edges recoil and spring open. This allows the healing factors to fill in and do their work to heal the wound. Essentially, these restrictions help contract the tissue, aiming to regain that previous level of tension needed to facilitate its necessary system-wide communication and functionality. Re-tensioning a pre-tensioned system is like cutting a rubber band. Without that tensile recoil, the rubber band might as well be just a string.
Turning Research into Practice
In our world of myofascial release, we are trained to push through the superficial tissue to access the “more important” deep fascia. In doing so, we bypass all the information the superficial tissue could be telling us. The same is true of a scar. A scar’s restrictions can be palpated superficially with light to moderate pressure (1–3 on the Walton Pressure Scale). The fascial restriction patterns have been found in conjunction with scars throughout the body in the same predictable pattern: Visualize it as a belt that is one notch tighter than the surrounding tissue, subtly compressing everything it surrounds.

The theory is that the body is protecting the injured area with these lines and bands. As a result, we need to ensure a level of safety with our touch from the start. You’ll note that the tissue around restrictions might respond to our hands-on work, but the protective pattern itself does not. After the restrictions feel they have been “released,” then we can do deeper work in the area. Overall, the message here is to start light to gain the trust of the brain and body. It may take a few sessions for the nervous system to trust that it can safely release the restrictions. Even after they have “released” to the point where the tissue is more functional, you can still feel them with palpation.
The patterns can be palpated to assess and locate; they feel deep to the dermis and superficial to the muscle/deeper fascia. However, where these lines overlap with the septa of muscle bellies and compartments, you can typically find adhesions. These add up to a restriction that runs the circumference of the injured limb and/or trunk (Image 3A). They are easy to miss, but once you attune your palpation, you can more readily find them. At times, you can see indents or wrinkles in the tissue, identifying where they are (Images 3B–E). If you cannot feel them, you need to remember the pattern, as if it were a map to help you navigate. These restrictions respond preferentially to gentle, slow, myofascial release techniques, as a way of working with the body’s inherent protective mechanisms of the nervous system.
The deeper and wider the scar, the more support it will need, especially bone-deep scars. Stability of the surrounding musculature, the level of atrophy, and the overall stress level of the client will determine if the body allows the restrictions to be released. High systemic stress or instability may inhibit release of these protective restrictions. Remember, we are working with a body and nervous system that both want to protect a vulnerable area, so don’t force it, and listen to what the client’s body tells you as you work to calm the protective mechanisms and release the restrictions.
Conclusion
While some restrictions may resolve gradually, others can persist for decades, potentially contributing to secondary complications such as spasms, weakness, altered sensation, lymphatic disturbances, idiopathic/complex/chronic pain, and/or additional surgeries. It is also common not to be bothered by the scar for several years, yet the scar is quietly pulling and impacting the overall structure, adding increased vulnerability to subsequent injuries.
It is my understanding that this protective pattern can still be felt in scars from surgeries conducted over 40 years ago. This theory has helped numerous clients and helped me zero in on their issues with less effort, aiding in the longevity of my career. Mapping these patterns can guide clinicians in expediting client rehabilitation and extending their own careers by minimizing exertion. My stance is that we therapists are already attenuating these restrictions with the work we are doing. The presentation of these lines as a map can help us be more strategic in modulating them to help expedite the client’s improved range of motion.
Notes
1. Nancy K. Smith and Catherine Ryan, Traumatic Scar Tissue Management, 1st ed. (Handspring Publishing Limited, 2016), 80–9.
2. Smith and Ryan, Traumatic Scar Tissue Management, 1st ed.; Colin Armstrong, “Unity, Continuity, Structure, and Function. The Ongoing Search for a Deeper Understanding of the Many Roles Attributed to Fascia in the Living Human Body—An Osteopathic Perspective,” OBM Integrative and Complementary Medicine 6, no. 3 (August 2021): 96–110, https://lidsen.com/journals/icm/icm-06-03-026.
3. Bessel van der Kolk, The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma (Viking, 2015).
4. Smith and Ryan, Traumatic Scar Tissue Management, 1st ed.
5. David Lesondak, Fascia, Function, and Medical Applications (CRC Press, August 2020).
6. Johns Hopkins Medicine, “Common Surgical Procedures,” accessed August 2025, https://hopkinsmedicine.org/health/treatment-tests-and-therapies/common-surgical-procedures.
7. Smith and Ryan, Traumatic Scar Tissue Management, 1st ed.
8. Smith and Ryan, Traumatic Scar Tissue Management, 1st ed.; Joanne Avison et al., “Chapter 3,” “Chapter 4,” “Chapter 7,” “Chapter 9,” and “Chapter 10,” Scars, Adhesions and the Biotensegral Body: Science, Assessment and Treatment, eds. Jan E. Trewartha and Sharon L. Wheeler (Handspring, 2020).
9. Carla Stecco et al., Functional Atlas of the Human Fascial System (Churchill Livingstone, 2015), 1–50, 289–366; Avison et al., Scars, Adhesions and the Biotensegral Body: Science, Assessment and Treatment; Armstrong, “Unity, Continuity, Structure, and Function. The Ongoing Search for a Deeper Understanding of the Many Roles Attributed to Fascia in the Living Human Body—An Osteopathic Perspective.”
10. Avison et al., Scars, Adhesions and the Biotensegral Body: Science, Assessment and Treatment.
11. Avison et al., Scars, Adhesions and the Biotensegral Body: Science, Assessment and Treatment.
12. Avison et al., Scars, Adhesions and the Biotensegral Body: Science, Assessment and Treatment; Armstrong, “Unity, Continuity, Structure, and Function. The Ongoing Search for a Deeper Understanding of the Many Roles Attributed to Fascia in the Living Human Body—An Osteopathic Perspective.”
A Deeper Dive—“A Hypothesized Bio-Tensegral Model for Scar Tissue, Observed in Anterior Cruciate Ligament Reconstruction Surgeries: A Case Report Series”
Here is a synopsis of my research findings, first presented at the 2022 Fascia Research Congress:
Purpose: Does a scar’s tissue engagement extend beyond the scar itself? I theorized that scar tissue affects areas beyond the immediate scar, engaging predictable lines of restriction within the soft tissue, even years after surgery. My research aimed to observe the existence of these restrictions across different participants and assess outcomes after myofascial release on the hypothesized pattern.
Participants: My observation of this pattern was bolstered by the case studies of 10 clients who had ACL reconstruction surgeries. The clients, ranging in age from 20 to 70, were between eight weeks and 10 years after surgery. They were still reporting limited active range of motion (AROM) and had previously had active lives before the injury and reconstructive surgery.
Intervention: Each client received five 50-minute sessions of light to medium myofascial release techniques (1–3 on the Walton Pressure Scale). The hypothesized restrictions were palpated at
each session.
Results: Restrictions were found in every client’s postoperative knee, showing the same patterns. After five sessions, clients exhibited an increase in AROM for flexion and extension. They also experienced less pain and guarding and improved circulation, proprioception, and balance.
Conclusion: This fascia engagement could explain the limb’s restriction of AROM. The restrictions appear to pin down all structures in their path in alignment with the scar’s location, potentially enabling:
-
New channels for a secondary retinacula/localized protection, giving real-time biofeedback to monitor and stabilize the structure
-
The re-establishment of a pre-tensioned
fascia system and assistance in wound healing and closure, in accordance to principles
of biotensegrity
A Scar’s Trauma Story
The initial training for massage therapists and bodyworkers often emphasizes cross-fiber friction and tissue mobilization techniques when working with scar tissue. But, it is essential to appreciate the broader impact of scarring on clients. From life disruptions, doctor’s appointments, financial burdens, and everything else that may come with injury and surgery, the postoperative massage clients we see may be handling a lot. The holistic consideration of the client behind each scar is paramount. Every scar has a story.
“We have learned that trauma is not just an event that took place sometime in the past; it is also the imprint left by that experience on mind, brain, and body. This imprint has ongoing consequences for how the human organism manages to survive in the present,” writes Bessel van der Kolk in The Body Keeps the Score.1
Emotional responses may surface during this work, especially if the therapist is the first to address the scar tissue. The physiological and psychological imprint of trauma literally rewires the brain; the impact may persist within the body long after the incident. Scar tissue warrants careful attention and sensitivity.
Note
1. Bessel van der Kolk, The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma, (Viking, 2015).









